Osteoarthritis, another name for osteoarthrosis, is a degenerative condition of the articular cartilage that is not inflammatory. It is characterized by:
- Thinning and destruction of articular cartilage
- Formation of osteophytes
- Capsular fibrosis
Etiology:
There is still much to learn about the precise cause of osteoarthritis. Its growth and advancement have been explained by a number of things.
Age: One of the main risk factors for osteoarthritis is getting older. Normal wear and tear on the cartilage caused by aging might cause the cartilage to break down. This may result in pain, stiffness, and restricted movement when the bones rub against one another.
Genetics: Osteoarthritis is also partially influenced by genetics. Osteoarthritis may also develop as a result of hereditary defects in the structure and makeup of cartilage and other joint components.
Obesity: An additional significant risk factor for osteoarthritis is obesity. Carrying too much weight puts extra strain on the joints, especially the hips and knees. Osteoarthritis may develop more quickly as a result of the accelerated cartilage loss. Furthermore, pro-inflammatory cytokines released by adipose tissue may aggravate and aggravate joint inflammation.
Trauma: Osteoarthritis can also result from trauma and injuries to the joint. This can include repetitive stress injuries from jobs requiring repetitive motions as well as injuries sustained in sports or accidents. Osteoarthritis can gradually develop as a result of these injuries, which can harm the cartilage and other joint structures.
Hormonal abnormalities, joint misalignment, and certain illnesses including gout and diabetes are other contributing reasons.
Pathology of Osteoarthrosis:
The cartilage loses its ability to absorb stress and provide a smooth surface for joint movement when osteoarthrosis progresses, becoming thinner and less elastic. Chondrocytes, which are the cells that make up cartilage, become less active and generate fewer of the proteins that keep cartilage in good condition.
The body produces new bone in the joint to try to heal the damage caused by the loss of cartilage, but this can result in the production of osteophytes or bone spurs. Due to increasing strain and stress on the joint, the subchondral bone, which is located directly below the cartilage, also expands and becomes dense.
An further factor in the pathophysiology of osteoarthritis is joint inflammation. Inflammation and thickening of the synovial membrane, which lines the joint and secretes synovial fluid, can cause additional harm to the bone and cartilage.
All things considered, the pathology of osteoarthritis is defined by a complicated interaction of elements, such as the degeneration of cartilage, the development of bone spurs, alterations in the subchondral bone, and inflammation of the joints. Significant pain and impairment may result from these alterations, especially in weight-bearing joints including the spine, hips, and knees.
Clinical Features of Osteoarthrosis:
The following are the clinical features of osteoarthritis:
- Joint Pain: The pain that osteoarthritis produces in the affected joint is either a burning or dull ache. A period of inactivity, like waking up in the morning, may make pain worse; yet, moving may make pain better.
- Stiffness: Osteoarthritis frequently manifests as stiffness, particularly in the morning or after a period of inactivity. It’s possible that the stiffness will become more noticeable after extended standing or sitting.
- Reduced range of motion: The affected joint’s range of motion may be limited by osteoarthritis. This can make it challenging to carry out specific tasks, such reaching or bending.
- Swelling: One of the most typical signs of osteoarthritis is joint swelling or inflammation. The joint may get warm to the touch and seem red as a result.
- Crepitus: When the affected joint is moved, a popping or cracking sound known as crepitus may be heard. This is because of the loss of cartilage causing the joint surfaces to become rough.
- Muscle weakness: Because osteoarthritis reduces joint function, it can result in muscular weakness in the affected limb.
- Deformities: Joint abnormalities, such as the formation of bony growths (osteophytes) or misalignment of the joint, may arise in advanced cases of osteoarthritis.
It is significant to remember that each person and the afflicted joint may experience these symptoms differently in terms of frequency and severity. Additionally, some individuals with osteoarthritis may not exhibit any symptoms at all, even in the face of severe joint destruction
Diagnosis:
Imaging investigations, physical examinations, and patient histories are often used to diagnose osteoarthritis. In cases where a patient exhibits joint pain, stiffness, or edema, a doctor may suspect osteoarthritis. The doctor may take the following actions to confirm the diagnosis:
- Patient history: The patient’s complaints, such as the location and duration of joint pain, stiffness, and edema, will be questioned by the doctor. They could also ask about the patient’s past surgeries or injuries that might have accelerated the onset of osteoarthritis, as well as their family history and medical history.
- Physical examination: To evaluate the strength, stability, and range of motion of the afflicted joint, the physician will conduct a physical examination. They might also search for indications of inflammation or joint deformity.
- Imaging studies: Imaging tests, like MRIs and X-rays, can support the diagnosis of osteoarthritis. Joint injury, including cartilage loss and the formation of bony growths called osteophytes, can be seen on X-rays, but MRI scans can provide more precise images of the damage.
- Laboratory tests: Laboratory testing can rule out other illnesses that might cause similar symptoms, but they cannot diagnose osteoarthritis. For example, blood tests can assist in ruling out autoimmune diseases such as rheumatoid arthritis.
In general, a comprehensive medical examination is necessary to rule out other potential causes of joint pain and stiffness and to confirm the existence of joint damage in order to diagnose osteoarthritis. Patients can manage their symptoms and enhance their quality of life with the right treatment and management after receiving a thorough diagnosis.
Grading of Osteoarthrosis:
Osteoarthrosis in a joint can be graded according to radiographic findings. The Kellgren-Lawrence grading system, which divides osteoarthrosis into five groups based on X-ray findings, is the most widely used of the numerous grading systems for the condition.
The following is the Kellgren-Lawrence grading system for osteoarthritis on X-rays:
Grade 0: The joint appears normal with no evidence of osteoarthritis.
Grade 1: There is minor joint space narrowing and possible osteophyte (bony growth) formation.
Grade 2: There is moderate joint space narrowing and osteophyte formation. The joint is still considered mild to moderate.
Grade 3: There is significant joint space narrowing, osteophyte formation, and some bony remodeling. The joint is considered moderately severe.
Grade 4: There is severe joint space narrowing, extensive osteophyte formation, and significant bony remodeling. The joint is considered severe.
It is important that there is not always an exact correlation between the osteoarthritis grading system and the disease’s symptoms or functional limitations. While some people with more severe osteoarthritis may have minimal symptoms, others with milder cases may have noticeable ones. Furthermore, the grading system is only one tool for the diagnosis and treatment of osteoarthritis; physicians usually take into account a number of criteria, such as the patient’s medical history and the results of their physical examination, when deciding on the best course of action.
Differential Diagnosis:
- Rheumatoid arthritis
- Gout
- Fibromyalgia
- Spondyloarthropathy
- Ankylosis spondylitis
Treatment:
Medications:
- NSAIDs
- Acetaminophen
- Opioids
- Glucosamine and chondroitin sulfate
- Glucocorticoids
- Intra-articular injections
Medical procedures:
- Total joint replacement
- Joint lavage
- Debridement
PT Management of Osteoarthrosis:
The following are some physiotherapy techniques for managing osteoarthritis:
- Exercise: Frequent exercise can help increase strength, improve range of motion, and lessen joint discomfort and stiffness. For those with osteoarthritis, low-impact activities like walking, cycling, and swimming are frequently advised. For each patient, physiotherapists can create a customized workout program that is both safe and efficient.
- Manual therapy: Joint mobilization, soft tissue mobilization, and muscle energy techniques are examples of manual therapy procedures that can assist increase joint mobility and lessen discomfort. Those with hip or spine osteoarthritis may find these methods very beneficial.
- Heat and cold therapy: Pain and stiffness in the affected joint might be lessened by applying heat or ice. While cold might assist relieve inflammation, heat can help enhance blood flow to the joint. A physiotherapist can advise on the right application temperature and duration of time for each patient.
- Assistive devices: Canes, walkers, and braces are examples of assistive technology that can help decrease joint stress and increase stability. A physical therapist can assist in determining which assistive technology is suitable for each patient.
- Education: Physiotherapists can instruct patients on ways to safeguard their joints, like pacing exercises, avoiding repeated motions, and maintaining good posture. By doing this, you may lessen joint stress and stop the afflicted joint from getting worse.
- Weight management: Reducing joint stress and increasing mobility can be achieved by maintaining a healthy weight. A physiotherapist can offer guidance on safe exercise routines and nutritious food choices to help with weight management.
All things considered, physiotherapy may be a successful osteoarthrosis treatment option. A physiotherapist can help patients manage their symptoms and enhance their quality of life by creating a personalized treatment plan that takes into consideration their particular needs and goals.
Exercises For Osteoarthrosis:
WHY EXERCISES?
- Exercises are mostly done to increase muscle strength.
- Because muscles are the dynamic stabilizers of the joint, a weak muscle will cause the joint to lose its stability.
- Because muscles power joints, a weaker muscle group will prevent the joint from producing the movements needed for daily activities.
- Therefore, increasing muscle strength continues to be a key component of therapy in order to enhance joint stability and mobility.
PROGRESSION OF EXERCISES:
- Isometric exercises
- Close kinetic chain exercises
- Open kinetic chain exercises
- Stretching exercises
- Conditioning exercises
Isometric Exercises:
These exercises are taught to the patient irrespective of the stage (mild/moderate or severe)
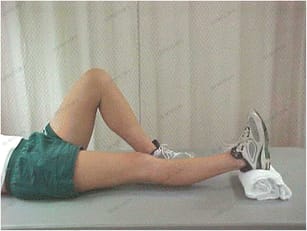
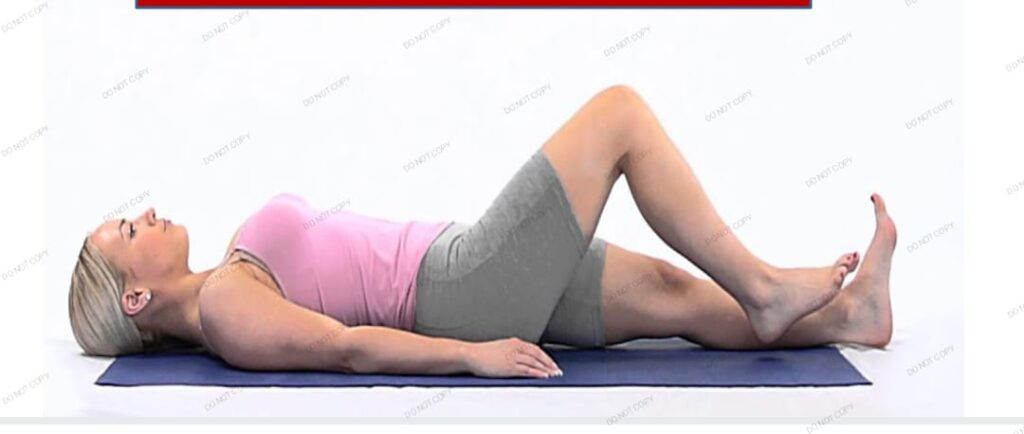
Lie with your legs straight on the floor. Press the towel with your knee joint after placing a towel roll beneath your knee. Repeat the press ten times with one leg, holding it for ten seconds each time.
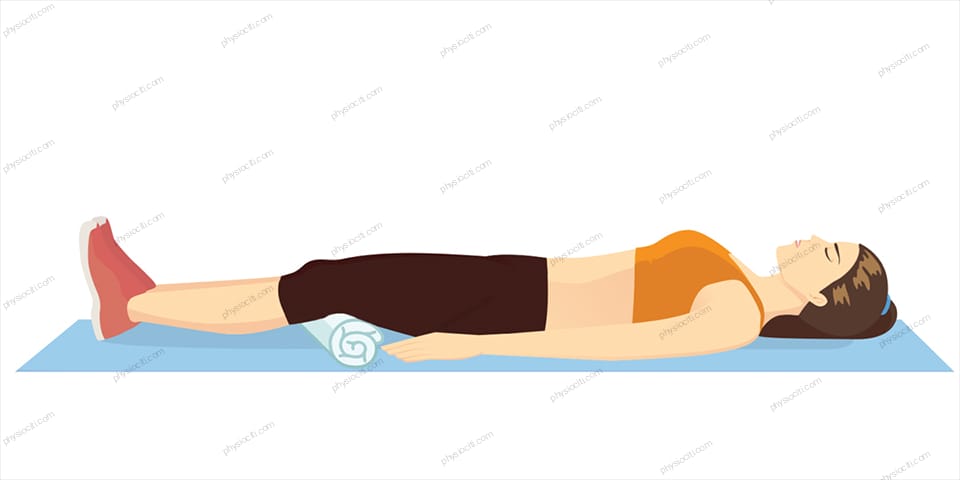

This time, position the towel roll below your ankle and press the towel toward the floor with your ankle. Repeat ten times, holding for ten seconds each time.
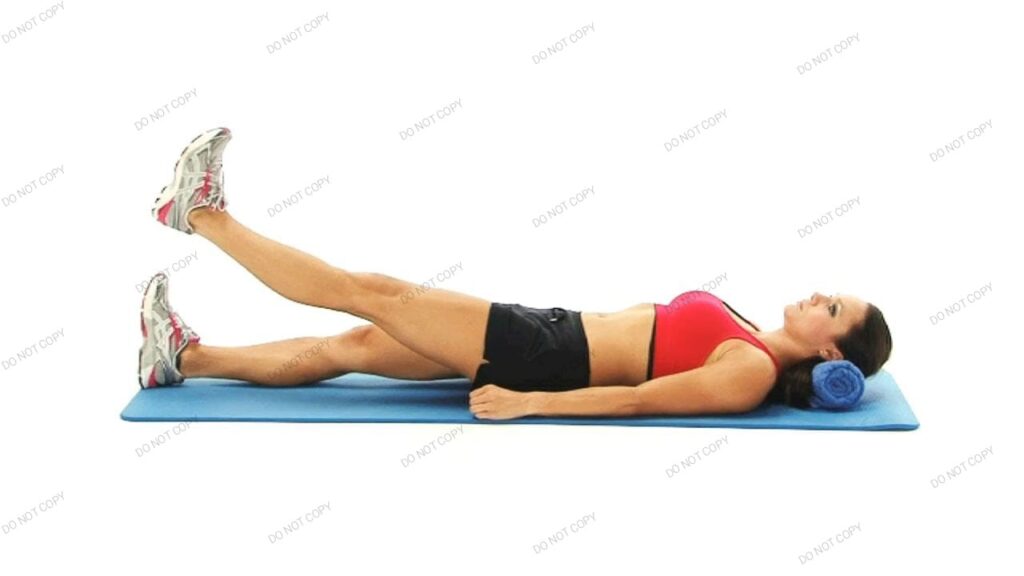
On the ground, lie down. Lift and hold your leg 30 to 40 degrees off the ground for a duration of 10 seconds. Repeat ten times.
Place your affected leg up and lie on your side. Lift the leg straight off the ground and maintain that position for ten or so seconds. Repeat ten times.

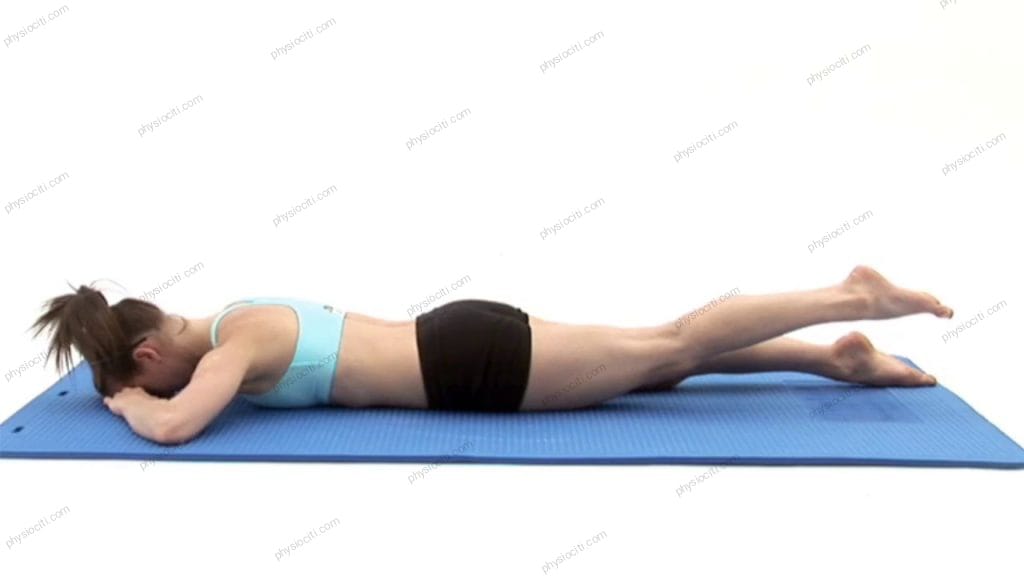
Place yourself on your stomach. Straighten your leg out to a height of 25 to 30 degrees, then hold it there for ten seconds. Repeat ten times.
Close Kinetic Chain Exercises:
Squat down till your thighs are parallel to the floor while standing up against a wall. Avoid deep squatting.


The vastus medialis oblique, or VMO, is an anterior thight muscle. It is essential to strengthen this muscle in order to manage osteoarthrosis.
To do this, perform a wall squat while pressing a ball or towel roll between both of your knees. Keep the ball in play. For approximately ten seconds, hold the ball or towel roll between your knees.
You can also accomplish this by sitting on a tall stool. To perform this, squat on a tall stool with your knees bent 90 degrees. With both hands, grasp the towel roll between your knees. Dorsiflex your ankle and extend one leg straight out while clutching the towel. For ten seconds, keep the leg raised in the air.

Isotonic Exercises:
Lie down on the ground, both legs extended. Now, slowly bend and then straighten one leg ten times or so. Use both legs while doing this.
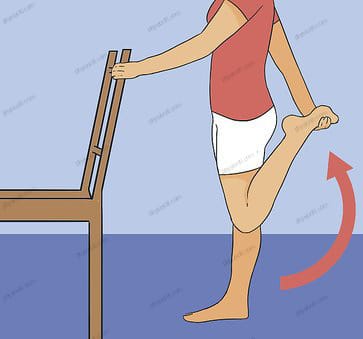
Take a seat as indicated by the image below. Lift and keep the leg straight up against the floor for a duration of five to ten seconds. This is going to raise resistance.

Stretching Exercise:


Conclusion:
In conclusion, millions of individuals worldwide suffer with osteoarthritis, a common degenerative joint condition. Although the precise etiology of the illness is still unknown, there are a number of risk factors that raise the chance of contracting it. Despite the lack of a cure, treatment techniques can lessen symptoms and enhance quality of life. For an accurate diagnosis and course of treatment, it’s critical to speak with a healthcare provider if you think you might have osteoarthritis.
ALSO READ- What is Carpal Boss Syndrome/ Os Styloideum?

Pingback: What is Carpal Boss Syndrome/ Os Styloideum? - ILLnessAid